Stay Ahead of the Curve
Latest AI news, expert analysis, bold opinions, and key trends — delivered to your inbox.
Generative AI in Mental Health: Diagnosing Schizophrenia and Predicting Long-Term Outcomes
6 min read Generative AI shows potential in diagnosing and predicting the progression of schizophrenia by analyzing mental health data for early detection and personalized care. However, concerns about misdiagnosis, bias, and privacy issues highlight the need for careful use alongside human expertise. April 07, 2025 07:48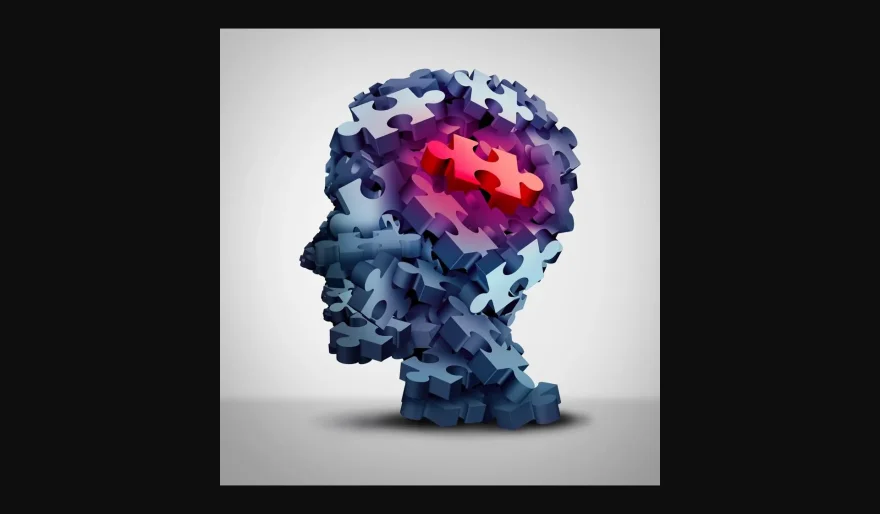
Schizophrenia is a complex and often misunderstood disorder, and while traditional diagnostic methods have made strides, there remains a gap in personalized, accurate prediction for long-term outcomes. Generative AI, however, offers a potential breakthrough in both diagnosing schizophrenia and predicting future health outcomes for individuals diagnosed with this condition.
Recent advancements have allowed AI models to analyze a wide array of mental health data, including clinical assessments, speech patterns, behavioral data, and neuroimaging scans. These models can detect subtle signs of schizophrenia that may not be immediately apparent to clinicians, thus offering earlier detection and more personalized treatment plans.
But the real promise of this AI application lies in its ability to forecast long-term outcomes. By analyzing historical data from patients with similar conditions, generative AI models can predict the progression of schizophrenia, such as the likelihood of hospitalization, response to treatments, and potential changes in cognitive and emotional health. These predictive capabilities could revolutionize how we approach mental health care, shifting from reactive treatments to more proactive, personalized care plans.
Broader Implications and Ethical Concerns
While the potential is compelling, the use of generative AI in mental health diagnosis and long-term prognosis raises several crucial ethical and practical concerns. There are risks of misdiagnosis or bias in AI models, which could lead to incorrect treatment plans or predictions. Furthermore, as AI takes a more prominent role in mental health, there are privacy issues related to the sensitive nature of the data being used.
These concerns underscore the importance of collaboration between AI experts, clinicians, and mental health professionals to ensure that the technology is used responsibly and effectively. Moreover, as AI continues to evolve, it will be essential to develop robust safeguards and ethical frameworks to prevent misuse and ensure patient well-being.
Previous Work and Broader Context
In my previous columns, I have explored numerous facets of AI in mental health, including how AI-powered mental health chatbots have become more integrated into therapy practices, assisting with patient engagement and providing immediate support outside of traditional therapy settings. AI’s role in enhancing the client-therapist relationship has been a topic of great interest, particularly regarding its ability to assist with personalized guidance and support between sessions.
Additionally, I’ve covered the autonomous guidance that generative AI can provide in therapeutic contexts, and examined global health reports such as those from the World Health Organization (WHO), highlighting the intersection of mental health care and generative AI on a global scale.
In case you missed it, I was honored to be interviewed in a CBS 60 Minutes episode that explored the rapidly evolving landscape of AI in healthcare. The episode provides valuable insights into AI’s transformative role in healthcare, including in the mental health space. You can find the full coverage here.
Looking Ahead: The Future of AI in Mental Health
As AI’s capabilities in the mental health sector continue to grow, the future looks promising. We can anticipate more AI-driven tools that not only assist in diagnostic accuracy but also offer ongoing predictive insights into patient progress. These advancements could drastically improve patient outcomes by enabling more tailored and timely interventions.
However, it will be critical to continue monitoring AI’s impact in mental health, ensuring that the technology serves as a supportive tool for clinicians, rather than replacing human expertise. Human judgment, empathy, and understanding will remain irreplaceable aspects of mental health care, and AI should be used to enhance these qualities, not diminish them.
Stay tuned for more updates on the cutting-edge use of generative AI in mental health as I continue to track its integration into healthcare practices and its broader implications for the future of treatment.








 AI Agents
AI Agents